Chorioamnionitis is an acute inflammation of the amniochorionic membrane, which can be caused by a bacterial infection. It is a significant cause of maternal and neonatal morbidity and mortality. Chorioamnionitis is associated with many short-term and long-term neonatal complications, including premature birth, neonatal sepsis, and cerebral palsy. The risk of chorioamnionitis is increased by premature rupture of the membranes and prolonged labour.
Artificial rupture of membranes (AROM) is a procedure used to intentionally rupture the chorioamniotic membranes to induce or augment labour. AROM is commonly performed during labour management and has been used by obstetric providers for hundreds of years.
AROM can be performed with a rod-hook device or a finger cot with a hook on the end. The hook is used to tear the amniotic membrane, and successful rupture is typically determined by the immediate return of amniotic fluid.
There is some debate about the appropriate timing of AROM to balance the risk of infection with the benefits of expedited labour induction. A study of nulliparous women undergoing induction of labour found that early AROM (at 4 cm) shortened time to delivery without increasing the risk of infection. However, another study found that early AROM increased the time to delivery and the risk of a caesarean section.
| Characteristics | Values |
|---|---|
| Definition | Inflammation of the amniochorionic membrane |
| Cause | Bacterial infection |
| Frequency | 1-10% of all pregnancies |
| Risk Factors | Increased number of vaginal examinations, duration of ruptured membranes, use of internal fetal monitors, coitus during pregnancy, bacterial colonisation, premature rupture of membranes, premature labour, invasive procedures |
| Symptoms | Fever, uterine tenderness, foul-smelling amniotic fluid, maternal and fetal tachycardia |
| Diagnosis | Clinical, microbiological or histopathological |
| Treatment | Antibiotics, antipyretics, expedited delivery, supportive care |
What You'll Learn
- Chorioamnionitis is an inflammation of the amniochorionic membrane, caused by a bacterial infection
- Chorioamnionitis is associated with many short- and long-term neonatal complications
- Chorioamnionitis is the most common obstetric cause of maternal sepsis
- Chorioamnionitis can occur with intact membranes
- Chorioamnionitis is a common complication of pregnancy

Chorioamnionitis is an inflammation of the amniochorionic membrane, caused by a bacterial infection
Chorioamnionitis is a serious condition that can occur during pregnancy, typically in the setting of prolonged membrane rupture or labour. It is an acute inflammation of the amniochorionic membrane, caused by a bacterial infection.
Chorioamnionitis is an infection that can occur before, during, or after labour. It can be acute, subacute, or chronic. The condition is caused by bacteria entering the tissues, membranes, or amniotic fluid surrounding a foetus, which can occur through an ascending vaginal infection, or less commonly, through hematogenous/transplacental spread or direct inoculation through invasive procedures. The most common bacteria that cause chorioamnionitis are E. coli and group B strep.
Chorioamnionitis is associated with many short- and long-term complications for both mother and foetus. Maternal complications include postpartum infections and sepsis, while adverse infant outcomes include stillbirth, premature birth, neonatal sepsis, chronic lung disease, and brain injury leading to cerebral palsy and other neurodevelopmental disabilities.
The diagnosis of chorioamnionitis is based on a combination of clinical, laboratory, and/or histopathologic findings. The key clinical findings include fever, uterine tenderness, maternal and fetal tachycardia, and foul-smelling amniotic fluid.
The treatment of chorioamnionitis involves antibiotics, and in some cases, early delivery. Antibiotics are typically given intravenously, and in the case of a Caesarean delivery, clindamycin is often added for anaerobic coverage.
The Aromatic Allure of Bluebird Fragrances
You may want to see also

Chorioamnionitis is associated with many short- and long-term neonatal complications
Short-term complications
- Perinatal death
- Asphyxia
- Early-onset neonatal sepsis
- Septic shock
- Pneumonia
- Intraventricular hemorrhage
- Cerebral white matter damage
- Respiratory distress syndrome
- Bronchopulmonary dysplasia
- Necrotizing enterocolitis
- Infections such as dermatitis and otitis media
- Poor response to surfactant
Long-term complications
- Cerebral palsy
- Brain injury
- Retinopathy of prematurity
- Chronic inflammatory disorders
- Increased vulnerability to infection
- Speech delay
- Hearing loss
- Schizophrenia
- Autism-specific phenotypes
- Chronic lung disease
- Neurodevelopmental disabilities
- Bronchopulmonary dysplasia
- Respiratory morbidity
- Asthma
Air Aroma: Ears Open or Shut?
You may want to see also

Chorioamnionitis is the most common obstetric cause of maternal sepsis
Chorioamnionitis is an acute inflammation of the membranes and chorion of the placenta, typically due to ascending polymicrobial bacterial infection in the setting of membrane rupture. It is a common complication of pregnancy, affecting 1-4% of all births in the US. Chorioamnionitis is the most common obstetric cause of maternal sepsis and is associated with significant maternal, perinatal, and long-term adverse outcomes.
Maternal complications of chorioamnionitis include postpartum infections and sepsis, postpartum hemorrhage, wound infection, pelvic abscess, bacteremia, and endometritis. Chorioamnionitis in a previous pregnancy may not be associated with an increased risk of chorioamnionitis in a subsequent pregnancy.
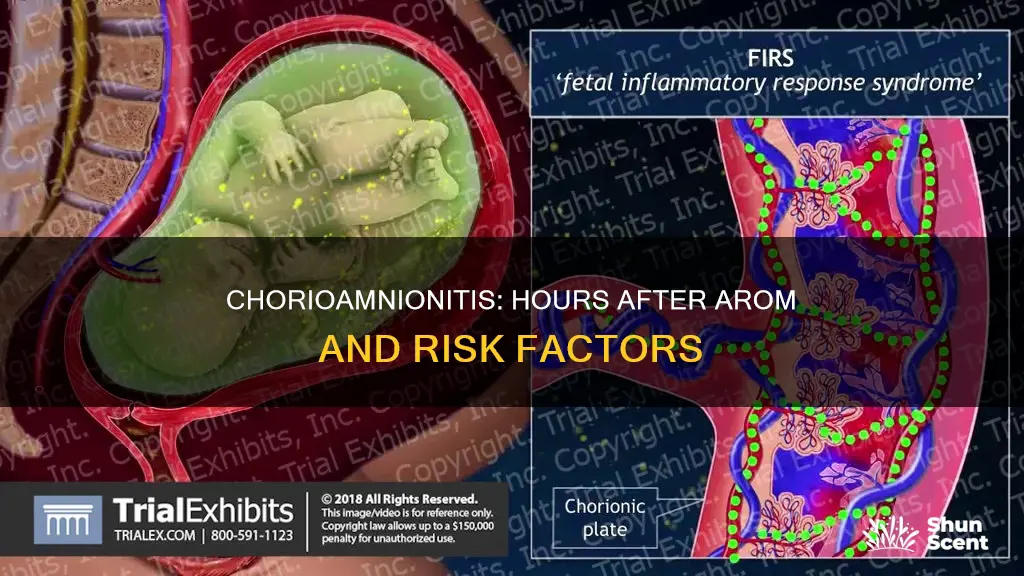
Fetal complications of chorioamnionitis include fetal death, neonatal sepsis, pneumonia, intraventricular hemorrhage, cerebral white matter damage, and long-term disability including cerebral palsy. The fetal response to infection is termed the Fetal Inflammatory Response Syndrome (FIRS) and may cause or aggravate some of these complications.
The Life and Times of Noel Aroma
You may want to see also

Chorioamnionitis can occur with intact membranes
Chorioamnionitis is an acute inflammation of the membranes and chorion of the placenta, which can occur with intact membranes. It is typically caused by a bacterial infection, with an ascending polymicrobial infection being the most common. Chorioamnionitis is associated with significant maternal and neonatal morbidity and mortality.
Chorioamnionitis is usually the result of an ascending infection from the lower genital tract, particularly in cases of premature rupture of membranes and prolonged labour. However, it can also be acquired through hematogenous/transplacental spread, or iatrogenic infection from amniocentesis or other invasive procedures.
The diagnosis of chorioamnionitis is primarily clinical, with fever being the most important clinical sign. Other clinical signs include uterine tenderness, foul-smelling amniotic fluid, and maternal and fetal tachycardia.
The treatment of chorioamnionitis involves antibiotic therapy, antipyretics, and the expedition of delivery. Antibiotics such as ampicillin and gentamicin are commonly used, with additional antibiotics added for anaerobic coverage in cases of a caesarean section.
Aromatherapy Safety: Pregnancy and Essential Oils
You may want to see also

Chorioamnionitis is a common complication of pregnancy
Chorioamnionitis is associated with many short- and long-term neonatal morbidities that cause a significant burden of disease on society. These include premature birth, neonatal sepsis, chronic lung disease, brain injury, and cerebral palsy. Chorioamnionitis is also the most common obstetric cause of maternal sepsis.
The key clinical findings associated with clinical chorioamnionitis include fever, uterine tenderness, maternal tachycardia (>100/min), fetal tachycardia (>160/min) and purulent or foul amniotic fluid. Fever is present in almost all cases of clinical chorioamnionitis and is considered the essential criterion for clinical diagnosis.
The diagnosis of chorioamnionitis is challenging due to a lack of consistency in diagnostic criteria, which may vary by provider and institution. It is typically made based on a constellation of clinical, laboratory, and/or histopathologic findings.
The most common complication of artificial rupture of membranes (AROM) is prolapse of the umbilical cord. This invariably occurs after rupture if AROM is performed when the head is not engaged in the maternal pelvis. In the case of an unengaged fetal head, the rupture of membranes may allow for the umbilical cord to precede the fetal head, generally leading to fetal bradycardia and necessitating emergency cesarean section.
In a study by Parrish et al. (2018), early AROM was not associated with an increased risk of chorioamnionitis. However, early AROM was associated with an increased time from the start of induction to delivery and an increased risk of cesarean.
A/B Testing: When to Test Arom vs Prom
You may want to see also
Frequently asked questions
Chorioamnionitis is an acute inflammation of the membranes and chorion of the placenta, typically due to ascending polymicrobial bacterial infection in the setting of membrane rupture.
Risk factors for chorioamnionitis include longer duration of membrane rupture, prolonged labor, nulliparity, African American ethnicity, internal monitoring of labor, multiple vaginal exams, meconium-stained amniotic fluid, smoking, alcohol or drug abuse, immune-compromised states, epidural anesthesia, colonization with group B streptococcus, bacterial vaginosis, sexually transmissible genital infections, and vaginal colonization with ureaplasma.
Chorioamnionitis leads to a 2 to 3-fold increased risk for cesarean delivery and 2 to 4-fold increase in endomyometritis, wound infection, pelvic abscess, bacteremia, and postpartum hemorrhage.
The key clinical findings associated with clinical chorioamnionitis include fever, uterine fundal tenderness, maternal tachycardia (>100/min), fetal tachycardia (>160/min), and purulent or foul amniotic fluid.
Chorioamnionitis can occur at any time after AROM. However, it is important to note that the risk of chorioamnionitis increases with prolonged membrane rupture.